DCRI team earns their rest following overnight, weekend CRIS 4.5 upgrade
 |
|
DCRI user support team members (standing, left to right): Devery Donovan, William Hernandez, Richard Carter, Chuck Gibbs, Mukesh Khatri, Stacy Coleman, Eric Clark, Patricia Dutcher, (at table, left to right) Mike Lyons, Larry Logan, Sabrina Lindsay, Bertram Brown, and Tam Tran.
|
The CC Department of Clinical Research Informatics on Saturday, March 10, worked through the night and most of the day to successfully upgrade CRIS, the Clinical Research Information System, from version 4.0 to 4.5. Five of the 52 people working on the project, including contractors, Eclypsis, and CC staff, arrived at 2:30 a.m. to begin working on the upgrade, which lasted 15 hours.
More than a one-day event, the upgrade required months of effort to configure the upgrade and rehearse it in January. CRIS enhancements are some of the largest projects for the DCRI team. User support staff spent the weekend upgrading every standard clinical desktop and the SunRay computers within Building 10 so users could access the improved system. In addition, DCRI support staff, provided 24-hour support from March 10-13, including staffing the help desk and visiting units to answer questions.
Susan Houston, chief of DCRI's project management office, said that the new features "will make it easier for users to accomplish certain tasks." Under the patient list tab, the changes include a forced patient selection; a one-click button to select all patients; and a color visual aid for improved readability of patient data. Under the orders tab, staff will see a new "alternate" tab, which will be used with the new pharmacy application expected to be implemented in early 2008. A final validation prior to submitting orders shows the name of the selected patient and also serves as an additional verification for patient safety. Under the documents tab, the "next" and "next section" buttons in the lower right-hand corner allow for easier navigation through the document sections. A print button allows users to print on-screen text for reference only.
CRIS users may contact the CRIS help desk at 301-496-8400 with questions about upgrade. Although the 4.5 upgrade does not require additional classroom training, the training materials have been updated with the additional features and new screenshots.
Back to Top
CC volunteers shine, inspire by example
Each year, the CC Social Work Department honors volunteers during National Volunteers Week, April 15-21. Sponsored by the Points of Light Foundation, the week thanks one of America's most valuable assets "our volunteers" and calls attention to all that they do to improve our communities. The 2007 theme, "Inspire by Example," reflects volunteers' power to inspire the people they help and inspire others to serve.
 |
CC volunteers (from left) Natalia Diaz-Rodriguez, Kirsten Newhams, and Silvia Ligorria
|
Volunteering at the CC inspires Kirsten Newhams, a pre-medical/post-baccalaureate student at American University, to persevere toward her goal of becoming a physician and teaches her about medical conditions, advances in medicine, research techniques, patient care, and how significant it is to make a connection with patients. Newhams and her classmate Natalia Diaz-Rodriguez began assisting with Spanish interpreting about six months ago because of their interest in multilingual medical settings. Diaz-Rodriguez agrees that the CC provides a unique learning environment for volunteers. "Doctors, nurses, social workers, and other CC staff are always eager to help and educate volunteers. Patients are a real joy to work with and they have taught me a lot about patience and perseverance," Diaz-Rodriguez said. "The health-care providers at the CC are so dedicated to what they do and it?s amazing to see the consistent attempts to go beyond the expected," Newhams said.
Silvia Ligorria began volunteering at the CC in 2005 after her son, Pedro, received treatment for a life-threatening disease. She visits mostly Spanish-speaking families because she understands what it's like to live "in a different culture in one of the most difficult moments of your life and have no one to talk to." Ligorria said she has learned that "when you give a little time to the patients and families, you really receive so much in return as their love and acceptance."
Andrea Rander, director of volunteer and language interpretation services in the SWD, said Diaz-Rodriguez and Newhams serve as "goodwill ambassadors" for the CC's volunteer program, and Ligorria shines in ensuring patients' comfort and satisfaction. The volunteers in turn may draw inspiration from their CC mentors, who are willing to assist with their interests and academic careers.
Come celebrate the inspiration CC volunteers provide at this year's award ceremony April 16 from 4 to 6 p.m.
Back to Top
Interpreters lend voices, patient support
 |
|
(from left) Brenda Robles and Maria Elena Guzman
|
Brenda Robles, a Spanish interpreter since November in the CC Volunteer Services and Language Interpreters Program, which is part of the Social Work Department, knows first-hand what it means to lend a voice to someone who can't communicate. Robles, the child of immigrant parents, became an interpreter because of her experiences as a child accompanying her mother to visit doctors, banks, and utility companies to communicate for her.
"It's a lot of pressure as a child, when you don't have the skill, capacity, vocabulary, or even the emotional maturity to communicate for someone else. And in health care, it's even more critical because medical interpretation requires a specialized knowledge of medical and legal terminology both in English and the patient's language. You are dealing with matters of life and death," Robles said.
Robles is a California state-certified medical interpreter with experience in simultaneous interpretation, or speaking at the patient?s pace in the first person with about a three-second delay. The advantage is that the messages are delivered in real time and carry the same emotion and intensity as the patient and provider are experiencing, allowing them to interact directly and build teamwork and trust. "It's two people conversing shadowed by one voice," Robles said. "I don't add my own opinions or judgments to the encounter. I simply mirror the words, messages, and emotions that are being exchanged in the target language, all within seconds," Robles said.
At the CC, interpreters may be involved in any aspect of a patient's experience from the moment they walk in the door to facilitate understanding around their care and treatment. Common situations requiring interpretation include patient intake, informed consents, protocol enrollment, diagnosis, prognosis, medical interventions, and family conferences. In addition, language interpreters often facilitate informal interactions throughout Building 10, making the entire facility run more smoothly.
The CC's volunteer interpreter program has recruited, trained, and supervised hundreds of community and student volunteers to bridge the language gap between patients and caregivers. Spanish, French, Cantonese, Portuguese, and Vietnamese are the program's most requested languages. "The lives of countless patients and families have been enriched by staff and volunteers who provide language interpretation and other patient support services," said Social Work Department Chief Dr. Adrienne Farrar.
Maria Elena Guzman, program support specialist/scheduler, came on board in August. Guzman, who was born in New York City but raised in the Dominican Republic with Spanish as her native language, was referred to NIH because of her work as a federal court interpreter and her desire to move into health care. "It is a pleasure for me to make it possible to provide access to care for these people who might not otherwise have a voice." Guzman said. Her role is to process orders received over the phone or through CRIS for interpretation services and coordinate calendars, schedules, and assignments of staff and volunteer interpreters. All volunteers are tested, interviewed, and screened to be part of the pool, and are further divided into scheduled on-site and on-call volunteers.
Guzman and Robles said their favorite part of their jobs is providing services to patients who can't speak for themselves. "Sometimes patients are in pain and can't communicate how they are feeling to the physicians and staff. Here they know they will find someone to interpret for them," Robles said, adding, "At the CC you see people looking for hope. We become collaborators in their hope for cures, treatments, and a better tomorrow."
Back to Top
Retired NIH staffer sets donation record
 |
Dr. Susan Leitman (left), director of blood services, presented Cameron with a plaque thanking him for his donations while Glorice Mason, medical technologist and team leader of the donor room, processed his noteworthy draw.
|
Tom Cameron, who retired in 1994 after 31 years with NIH, set a record at the blood bank on March 9 with his 200th donation - all at our facility. Cameron, former chief of the Animal Hospital Section - now the intensive care unit of the Division of Veterinary Resources in the Office of Research Services - became NIH's 95th donor when he began donating in 1963. The blood bank now has more than 23,000 donors.
Back to Top
Robot, IMRI assist protocols in anesthesia, surgical services
The Department of Anesthesia and Surgical Services has two technological resources available to support clinical research—a robotic surgery system and an intra-operative magnetic resonance imaging suite. Because the CC’s mission is clinical research, this is not a typical surgery and anesthesiology department, said Dr. Zena Quezado, DASS chief and a specialist in critical care medicine and pediatric and cardiac anesthesia.
 |
|
NCI's Dr. Gennady Bratslavsky (at patient bedside), urologic oncology fellow, and Dr. Peter Pinto (standing by console) perform a robotic-assisted radical prostatectomy, while CC anesthesiologist Dr. Xiaowei Lu monitors the patient.
|
In 2005 NCI and the CC acquired the robotic surgery system. It is currently used for prostate and kidney cancer surgery, although investigators are considering additional applications. The da Vinci is a “tremendous leap forward and advancement in surgery,�? Dr. Peter Pinto, a surgeon in NCI’s Urologic Oncology Branch in the Center for Cancer Research, said, especially for traditional radical prostatectomies—the removal of the entire prostate gland and pelvic lymph nodes. The surgery without the robot requires an incision from belly button to the pubic bone, with two or three urologic surgeons’ hands inside the patient. A radical prostatectomy with robotic technology uses the same instruments, only they’re longer and function as an extension of the surgeon. During a surgery, Pinto sits on the other side of the suite from the patient, with his head tucked into a large console and his hands grasping controls that translate how he moves the “wristed�? surgical instruments. The robotic unit provides a super-magnified, three-dimensional image of the patient’s abdomen so the procedure becomes, in effect, a minimally invasive laparoscopic surgery performed with small “keyhole�? incisions in the lower abdomen. Laparoscopic surgeries use two-dimensional images and have no depth. The CC’s system allows for 3D viewing in the console, which emulates the open technique. The camera also magnifies the view to 10 to 15 times greater and can come within millimeters of the tissues being examined—something a surgeon could not do with the naked eye.
Pinto’s protocols are exploring the benefits of the relatively new technology by incorporating it into the operating room and tracking patient quality-of-life outcomes. “Urologic surgeons at large are offering [robotic-assisted radical prostatectomies] to patients across the country, so we thought it should be examined critically here,�? Pinto said. There is a trend toward improved patient outcomes with laparoscopic techniques in a few categories: pain and suffering after surgery, blood loss, and return-to-work rates, and some studies show the same benefits with robotic technology, according to Pinto. To track patient quality-of-life outcomes over time, Pinto’s patients respond to a validated questionnaire before surgery and one, three, six, and 12 months after surgery.
Pinto’s team on March 15 also completed the first robotic-assisted laparoscopic partial nephrectomy (LPN) in a patient with multiple renal tumors. The CC and NCI run protocols for patients with inherited forms of kidney cancers, which can produce multiple tumors in one or both kidneys in a lifetime. Instead of removing the kidneys, which would require dialysis and reduce quality and length of life, most surgeons remove tumors but leave the kidney intact through open surgery, which often requires removing the 11th rib and muscle.
The CC is one of the few places across the country offering LPN, which requires extensive training and surgical skills, but also provides the benefits of a minimally invasive procedure. However, it is still difficult to create a bloodless operating space and to remove multiple tumors with LPN. With a robotic-assisted procedure, Pinto could suture the highly vascular kidney faster to control bleeding and removed three tumors from the patient’s kidney. A Magnet in the OR
The IMRI suite, a collaborative effort that CC, NCI, and NINDS opened in 2005, provides real-time imaging during surgery and a display of current and pre-operative images using three-dimensional and virtual reality technology. Fewer than 20 facilities nationwide have high-field interventional IMRIs similar to the CC’s. It has a 1.5 Tesla magnet that allows staff to obtain better images.
 |
|
The power and complexity of the IMRI’s magnet required DASS to adapt on several levels. All the surgical instruments must be non-magnetic so they will not be attracted to and fused to the IMRI. Magnetic objects, such as pens or non-digital watches, aren’t allowed beyond the red line on the floor or they they could become projectiles. Gold and silver jewelry may be worn in the IMRI room. DASS created extensive policies and procedures for those entering through the thick wooden door (right) that seals the IMRI suite, including designating one staff member responsible for screening patients and staff for implanted devices. A pacemaker, for example, might be disrupted or reprogrammed by contact with the IMRI’s magnetic field. DASS trained its entire staff on how to safely work in an IMRI environment and developed procedures for how to screen staff quickly so they could enter the room in case of an emergency.
|
Quezado said one of the unique uses for CC’s IMRI is to track the infusion of solutions of enzymes and chemotherapeutic agents into the brain to treat metabolic diseases and brain tumors. Drs. Edward Oldfield, chief of neurosurgery at NINDS; Russell Lonser, staff clinician in the clinical neurosurgical section at NINDS; and ORS Division of Bioengineering and Physical Science bioengineers Robert Dedrick and Paul Morrison developed the infusion technology and brought it to the bedside in the CC for adult brain tumor patients and pediatric patients with Gaucher disease and brain stem gliomas. Dye is mixed with the medication so that it will show up in the machine’s images of the brain and allow staff delivering the agent to watch how it travels. Unlike a regular MRI that is performed periodically, the IMRI allows almost continuous scanning so the surgeons can track in real-time the distribution of the therapy.
The IMRI also allows surgeons to move seamlessly between operating and imaging, visualizing tumors before, during, and after an operation. For example, Dr. John Heiss, NINDS staff neurosurgeon, uses the IMRI during craniotomies, in which the skull is opened to remove tumors located close to the parts of the brain that allows one to understand speech. Heiss uses the IMRI to assist in approaching the tumor, pinpointing its border and nearby structures, monitoring how much tumor remains throughout surgery, confirming the removal of all abnormal tissue, and identifying other problems, such as blood clots, that must be addressed before ending the procedure. With the IMRI, surgeons can collect the information quickly, efficiently, and precisely during one operation rather than a succession of surgeries.
In addition to real-time tracking of therapies and tumor imaging, NIH researchers apply the IMRI to improving the effectiveness of other targeted therapies, such as radiation. For example, by imaging the upper abdomen and creating IMRI-based movies, physicians can see how the pancreas moves with respiration and can coach patients on how to breathe so their organs stay in the radiation field. Dr. Anurag Singh, an NCI staff clinician, currently uses the IMRI to study bowel and pancreas motion and target breast biopsies. “The nice thing about IMRI is that you don’t have any radiation, so patients can receive it over and over again,�? Singh said. The IMRI is valuable for populations, such as children, who should minimize radiation exposure throughout their treatment. According to Singh, the CC is unique because it is “one of the few places where you can get a magnet in the operating room.�?
Back to Top
William “Billy�? Washington leaves legacy of 42 years of service to CC oncology patients
 |
|
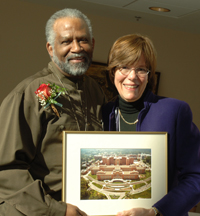
William “Billy�? Washington with Clare Hastings, chief of nursing and patient care services, at his CC retirement party on March 6.
|
William “Billy�? Washington, who started caring for NCI patients in 1964 when the Clinical Center was only 11 years old, retired in March after 42 years of service. When Washington passed the civil service exam and accepted a nursing assistant position at the CC that year, NCI was one of nine NIH institutes. He earned $4,000 annually. Caring for oncology patients with radical surgical disfigurements at that time was quite difficult, and Washington said he almost quit after his first month of training. To the benefit of his patients and the institution, given the tremendous need for caregivers, he did not.
Throughout the late 1960s, Washington worked on 13 East in the “Life Island�? laminar flow rooms. During his four-decade CC tenure, Washington witnessed many achievements and advancements in clinical oncology research and oncology patient care, assisted on every oncology unit, and worked with thousands of staff.
Washington said that caring for oncology research patients for 42 years has been a very humbling experience that made him appreciate the gift of life and good health every day. “NIH is not just for American health and research, but for all of humanity, to advance worldwide and global preservation of health,�? Washington said.
Washington is married to his soul mate, Lelia, and they are very proud of their two sons and 12 year-old granddaughter, Taylor Love. His son Marcus is a local Ebenezer African Episcopal minister with a Master’s from Howard University’s School of Divinity. Son De’Andre is an energetic teenager. Washington looks forward to playing golf, bowling, and dancing in his upcoming retirement years.
Washington’s colleagues say his strong work ethic and caring attitude have made him an exemplary coworker and peer to those fortunate enough to have worked with him. His patients continue to praise his many technical and personal caring skills, as they cope with frequent chemotherapies, radical surgeries, radiation, and recurrent medical problems. According to Betsy Wendell, the nurse manager on 3NE, “it takes a very positive, patient, and special person to care for oncology patients and to do so for 42 years. It is nothing less than heroic, outstanding, and truly amazing. Billy is an inspiration for all of us. You are a CC legend and your legacy will long be remembered by many at NIH. All the best to you, always.�?
Back to Top
Housekeeping aid Clifford Thomas retires after 52 years
 |
|
Clifford Thomas (left) stands with NIH Director Elias Zerhouni on May 25, 2005, at the HHS Secretary’s Departmental Honor Awards.
|
Housekeeping aid Clifford Thomas began working at NIH in February 1955, when Rockville Pike was just a three-lane road. “I used to drive by and see NIH and I wondered if I could get a job there,�? Thomas said. Since then, he worked in various places across NIH, most recently assigned to CC Director Dr. John I. Gallin’s suite. Thomas went on to receive his 50-year pin and a handshake from HHS Secretary Michael Leavitt and NIH Director Dr. Elias Zerhouni in 2005 at the HHS Secretary’s Departmental Honor Awards. Thomas retired from service on Feb. 28.
Gallin said Clifford “is one of those exceptional people who distinguish themselves through their actions and reliability. He’s remarkably dedicated, efficient, and pleasant. That he’s decided to stay on with us for so many years is certainly fortunate for us. His work ethic and values are greatly appreciated.�?
Back to Top
Two CC leaders head national societies
 |
|
Dr. Frederick P. Ognibene (left) and Dr. Henry Masur
|
Dr. Frederick P. Ognibene, director of the CC Office of Clinical Research Training and Medical Education, became the 37th president of the Society of Critical Care Medicine (SCCM) in February. “Being involved in the Society and its activities has offered me the opportunity to further develop my personal and professional education and commitment to the critical care field,�? said Ognibene. “It’s an honor to serve as the president of such a diverse and amazing organization, and I look forward to furthering its mission and vision during my term.�? With more than 13,000 members worldwide, the Society is the only professional organization devoted exclusively to the advancement of multi-professional intensive care through excellence in patient care, professional education, public education, research, and advocacy.
In addition, Dr. Henry Masur, chief of the CC Critical Care Medicine Department, is current president of Infectious Diseases Society of America (IDSA). IDSA represents about 8,000 infectious disease specialists and seeks to improve health by promoting excellence in infectious disease patient care, education, research, public health, and prevention. Dr. Masur said that “leading the IDSA provides an opportunity to improve clinical practice and advocate for sound public policy in areas that are vitally important to health in the U.S. and abroad.�?
Masur and Ognibene are both graduates of Cornell University Medical College, although they did not attend at the same time. Masur, together with former CCMD Chief Dr. Joseph Parrillo, in 1982 recruited Ognibene as one of the first four CC-trained critical care fellows. Their professional paths continued to be linked for 20 years; Ognibene became a tenured senior investigator in CCMD after completing his fellowship. Ognibene assisted Masur and his team with improvements in the critical care fellowship program, medical directorship of the department’s respiratory therapy staff, and with developing an organized data management system for CCMD’s HIV/AIDS research data and records, which resulted in many early studies on HIV/AIDS’ pulmonary and infectious disease complications.
Other CCMD physicians who have served as society presidents include Drs. J. Perrin Cobb, Society of Surgical Research; CCMD senior investigator Robert Danner, American Board of Internal Medicine’s Critical Care Medicine Test Committee; Jeffrey Dichter, Society of Hospital Medicine; Margaret Parker, SCCM; and Parrillo, SCCM.
Back to Top
Sculpture honors former CC nurse
 |
(from left): Bob Biddle, Susan’s brother; Diane Vollberg; Barbara Hansen, 5SES staff nurse; and Bobby Biddle, Susan’s sister-in-law, at the dedication.
|
Clinical Center staff gathered on March 7 at the 5SES entrance to view a sculpture by Washington artist Tim Tate honoring the memory of former CC nurse Susan Biddle. Biddle, who died in 2005, worked here for more than 20 years.
The sculpture’s location pays tribute to her specialization in cardiology, hematology, and sickle cell anemia patient care. Diane Vollberg, neurology clinic coordinator for OP7, where Biddle worked before she died, said family, friends, and staff voluntarily contributed to the purchase of the sculpture “so her name would continually be spoken at NIH.�?
Etched onto the sculpture, “In God’s Hands,�? are six words selected by CC staff to describe Biddle: humor, devotion, wisdom, compassion, integrity, and nurse.
Back to Top
Know your fluids
 |
|
Dietetic interns (from left) Kirsten Zambell, Shelly Falls, Shanna Bernstein, and Amber Courville
|
As part of March’s national nutrition month, volunteer dietetic interns (from left) Kirsten Zambell, Shelly Falls, Shanna Bernstein, and Amber Courville hosted a display table with posters, empty containers, and handouts about seven types of fluids: energy drinks, sports drinks, water drinks, juice and juice drinks, coffee and tea, milk, and sodas.
The display visited several patient care units—including 3NW, 5NW, 5SES, and 5SEN— throughout March to reach additional patients and CC staff.
Back to Top
Kids see physical therapy patient in action
 |
(from left) Students Jamie Palmer, Victor Ying, Tiffany Le, Anika Jain, and Rakhee Jain listen to CC patient Bernadia Lovely (far right) speak.
|
About 70 seventh grade students from Roberto Clemente Middle School’s math, science, and computer science magnet program in Germantown on March 8 toured the NIH Clinical Center’s Rehabilitation Medicine Department. They learned about the role physical therapy plays in patient rehabilitation and clinical research. The students also heard Lovely talk about her diagnosis with osteosarcoma, a pediatric cancer, and her experiences receiving chemotherapy and adjusting to life with a prosthesis. Lovely, a college art major, wants to become a cartoonist and works with an art therapist to express herself during her treatment. She’s also writing a book about her life, what she has learned, and how she has grown from her experience with cancer. “People think of having cancer as being the end of the world. But it’s not,�? Lovely said.
Back to Top
News Briefs
Deputy CIO named
Patricia Sengstack recently joined the CC Department of Clinical Research Informatics as deputy chief information officer. She will be a lead resource for members of the multidisciplinary care team that uses CRIS. As an application analyst for the Computer Science Corporation (CSC), she helped plan and implement CRIS activation activities from 2003 to 2005. Since August 2005 she has been CSC’s project support lead for many aspects of CRIS activation, including user account management, clinical documents, results retrieval, and business process redesign. Board certified in nursing informatics, Patricia earned her BS and MS in nursing from the University of Maryland and completed a post-master’s degree in nursing informatics there in 2002.
Spring brown bag series focuses on leadership development
The CC Office of Workforce Planning and Development has initiated a brown bag lecture series focusing on leadership development. Bring your lunch to 4-2551 from noon to 1 p.m. on the following dates and listen to coaches in the CC’s leadership coaching program address workplace topics. Space is limited, so please RSVP to Yasmin Coates at ycoates@cc.nih.gov or 301-402-5285.
April 16: “Five dysfunctions of a team and how to avoid them�?—Arleen La Bella
May 16: “Avoiding Karoshi (translation: death by overwork)�?—Cynthia Way
June 18: “Difficult Conversations: What the Harvard negotiation project can teach us�?—Paula Lowe
July 11: “Using the Myers-Briggs to improve team performance�?—Hany Malik
Pharmacy department hosts symposium
The CC pharmacy department on April 21 will host its annual symposium, Pharmacotherapy Frontiers. Topics include trends in rheumatoid arthritis treatment, the pharmacological basis of schizophrenia, FDA’s process for approving generic drugs, and preventing medical errors. An agenda and registration information are available online at www.cc.nih.gov/phar/.
CC celebrates nurses May 6-12
The CC and the American Nurses Association are proud to recognize the nearly 2.9 million registered nurses nationwide May 6-12. This year’s theme, “Nursing: A Profession and a Passion,�? emphasizes the commitment to patients that nurses share. Events at the CC will include:
May 7: Rear Adm. Carol Romano, chief nurse officer in the U.S. Public Health Service and deputy chief of DCRI, will speak at the opening ceremony from 10 a.m. to noon in Masur.
May 8: Visit an education workshop in the 1SE atrium from 8 a.m. to noon. Booths will focus on topics including therapeutic communication, pain assessment, conducting and appraising library research, learning assessment tools, and craft and relaxation therapy.
May 10: The education workshop returns to the 1SE atrium from noon to 4 p.m.
May 11: The 2007 team awards will be presented at the closing ceremony from 1 to 3 p.m. in Masur. A reception will follow.
New standards to guide patient care
The Medical Executive Committee’s “Standards for Patient Care at the NIH Clinical Center�? are now online at www.cc.nih.gov/ccc/patientcare/index.html.
Dr. Richard Cannon, NHLBI clinical director and former MEC chair, coordinated the preparation of the standards for the MEC. The standards cover:
• Credentialing and privileging;
• Pre-admission preparation;
• Multidisciplinary patient care rounds;
• Patient management and treatment guidelines;
• Patient discharge and referring physician interface;
• Quality assurance and quality improvement;
• Morbidity/mortality rounds; and
• Great teachers lectures and medical and ethics grand rounds.
The new standards complement MEC’s “Standards for Clinical Research Within the NIH Intramural Research Program,�? introduced in 2000, also online at www.cc.nih.gov/ccc/clinicalresearch/index.html.
Back to Top
New clinical research protocols
Molecular Changes and Biomarkers in Chronic Myeloproliferative Disorders, 07-CC-0090, David F. Stroncek, MD, CC
An Exploratory Study to Evaluate the Ability of Epigallocatechin Gallate to Simultaneously Improve Metabolic and Cardiovascular Actions of Insulin in Healthy, Obese, Hypertensive, or Diabetic Subjects, 07-AT-0089, Michael J. Quon, MD, NCCAM
A Natural History Study of HIV Acquired in Infancy or Childhood, 07-C-0087, Rohan Hazra, MD, NCI
A Phase I Study of Batracylin (NSC320846) in Subjects with Solid Tumors and Lymphomas, 07-C-0097, Martin E. Gutierrez, MD, NCI
Collection of Blood from Patients with Prostate Cancer, 07-C-0100, William D. Figg, PhD, NCI
A Phase 0 Trial of 111 Indium CHX-A DTPA Trastuzumab Imaging in Women with Stage I-IV Breast Cancer, 07-C-0101, Peter L. Choyke, MD, NCI
A Randomized Phase 2.5 Study of (153) Sm-EDTMP (Quadramet) With or Without a PSA/TRICOM Vaccine in Men With Androgen-Insensitive Metastatic Prostate Cancer, 07-C-0106, James L. Gulley, MD, NCI
A Randomized Phase II Trial Combining Vaccine Therapy with PROSTVAC/TRICOM and Flutamide, vs. Flutamide Alone in Men with Androgen Insensitive, Non Metastatic (D0.5) Prostate Cancer, 07-C-0107, Philip M. Arlen, MD, NCI
A Phase 1, Multicenter, Dose Escalation Study of CAT-8015 in Patients with Relapsed or Refractory Chronic Lymphocytic Leukemia (CLL), Prolymphocytic Leukemia (PLL), or Small Lymphocytic Lymphoma (SLL), 07-C-0108, Robert J. Kreitman, MD, NCI
Analysis of Stored Data Collected from Individuals Administered Neurobehavioral Assessments on IRB-Approved Protocols, 07-C-0110, Rohan Hazra, MD, NCI
A Pilot Study of Markers of Tumor Burden and Radiation Toxicity in the Blood, Urine, and Stool of Patients Receiving Radiotherapy for Gastrointestinal Malignancies, 07-C-0111, Deborah E. Citrin, MD, NCI
A Phase I Study of Subcutaneous CYT 107 (Interleukin-7) in Refractory Metastatic Melanoma or Renal Cell Carcinoma, 07-C-0114, Steven A. Rosenberg, MD, NCI
WTI Peptide Vaccination for Patients with High Risk Hematological Malignancies, 07-H-0091, Katayoun Rezvani, MD, NHLBI
A Phase II Study of Lenalidomide Revlimid® in Previously Treated Patients with Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma, 07-H-0104, Georg Aue, MD, NHLBI
Collection of Blood, Bone Marrow, and Buccal Mucosa Samples from Normal Volunteers, 07-H-0113, Neal S. Young, MD, NHLBI
Accuracy of Hemoglobin A1C to Predict Glycemia in HIV, 07-I-0094, Colleen M. Hadigan, MD, NIAID
Pioglitazone for Hepatic Steatosis in HIV, 07-I-0105, Colleen M. Hadigan, MD, NIAID
Back to Top
Upcoming events
April 4, 2007
Ethics Rounds
A Family’s Request for Complementary Medicine After Brain Death
Arthur Applbaum, Ph.D.
Professor of Ethics and Public Policy, John F. Kennedy School of Government
Director of Graduate Fellowships, Edmond J. Safra Foundation Center for Ethics, Harvard University
Lecture will be videocast, http://videocast.nih.gov
April 11, 2007
Great Teachers
Contemporary Clinical Medicine: Great Teachers
Mysterious Cases
Lawrence M. Tierney Jr., M.D.
Associate Chief, Medical Service, San Francisco VAMC
Professor of Medicine, University of California at San Francisco
Lecture will be videocast, http://videocast.nih.gov
April 18, 2007
Akt and TRAIL: The Yin and Yang of Targeted Cancer Therapies
Phillip A. Dennis, M.D., Ph.D.
Senior Investigator, Medical Oncology Branch, Center for Cancer Research, NCI
Stan Lipkowitz, M.D., Ph.D.
Senior Investigator, Laboratory of Cellular and Molecular Biology, Center for Cancer Research, NCI
April 25, 2007
Learning Some New Tricks From a Multidrug Transporter
Michael M. Gottesman, M.D.
Deputy Director for Intramural Research, NIH; and Chief, Laboratory of Cell
Biology, NCI
Imaging Efflux Transporter Function with Positron Emission Tomography (PET)
Robert B. Innis, M.D., Ph.D.
Chief, Molecular Imaging Branch, NIMH
Back to Top
Clinical Center News, National
Institutes of Health, Building 10, 10 Center Drive, Room 12C440, Bethesda, MD 20892-1504. Tel: 301-496-6787.
Fax: 301-402-2984. Published monthly for CC employees
by the Office of Communications, Patient Recruitment, and Public Liaison. News, article ideas,
calendar events, letters, and photographs are welcome.
Back to Top
|
|


 The information on this page is archived and provided for reference purposes only.
The information on this page is archived and provided for reference purposes only.