NIH staff honor trailblazer for 30 years as a hepatitis clinical research participant
 |
|
(back row, from left) Dr. Barbara Rehermann from NIDDK, Dr. Harvey Alter from the CC, Dr. T. Jake Liang from NIDDK, Dr. Robert Purcell from NIAID, Dr. Patrizia Farci from NIAID, and Dr. Susan Leitman from the CC. (front row) Kimiyo Hutchinson, William Hutchinson, and Cathy Schechterly from the CC. Hutchinson’s cake reads "Happy 30th to Mr. H. and his virus."
|
NIH staff celebrated an unusual birthday of sorts with William Hutchinson on July 25. He has contributed more than any other patient in the world to NIH researchers’ understanding of the hepatitis C virus. It was about 30 years ago that he contracted the virus, beginning a unique clinical research relationship with scientists around the globe. Although Hutchinson has attended lectures at NIH where researchers with a technical interest in his blood convened, this was the first time that he met the researchers who had pored over his cells.
Hutchinson, now 90, thinks it was his career of international travel and diplomacy that prepared him for these past three decades of his life and the resulting renown among medical researchers across the globe. Before he retired in 1973, Hutchinson served as a public affairs officer for the U.S. government in countless countries. His career highlights include editing General Douglas MacArthur’s reports to the world on the occupation of Japan and working in Hong Kong when President Richard Nixon went to China. He speaks multiple languages, including Arabic, Cantonese, Hindi, Punjabi, and Urdu. He estimates that he spent time in about 25 African countries, where he’d encounter indigenous infectious disease strains with every river and valley he crossed. Unbeknownst to him, Hutchinson’s immune system grew stronger and developed antibodies as he traveled the globe. "It did a remarkable job on my immune system to live in so many different places," Hutchinson said.
An avid hiker and mountain climber, Hutchinson first came to the NIH Clinical Center in April 1977 when he had a heart attack on a trail in New Hampshire. With his extensive government service, friends suggested that he might find treatment at NIH. He received 18 units of blood following his open heart surgery, and one of them was contaminated with what is now called hepatitis C, then known only as non-A/non-B hepatitis. There was no way to screen the blood supply for hepatitis at that time, because no screening test existed. Although the virus remains in his bloodstream, Hutchinson has no symptoms related to the infection, and liver biopsy has shown that he has had no disease progression in 30 years. Hutchinson’s immune system has contained the virus, but not eradicated it. Investigators continue to study this balance between virus and host.
 |
|
William Hutchinson donates blood through apheresis on July 25, the 30th birthday of his virus.
|
Dr. Harvey Alter, chief of the CC Department of Transfusion Medicine’s infectious disease section, said Hutchinson was the right patient at the right time in the right place. "Because he was being followed in an NIH protocol, we detected the onset of hepatitis very early in its course and obtained a plasma sample just when, as we later found, his virus was growing rapidly and was in its most infectious state," Alter said. Working closely with the lab of Dr. Robert Purcell in NIAID, Alter divided the plasma into vials to determine the titer of the virus, estimate its size and density, show that it had a lipid envelope and physically characterize the virus even before researchers knew what it was. Dr. Patrizia Farci from NIAID cloned the Hutchinson (H) strain virus and demonstrated that his viral agent contained a large family of closely related viral variants, rather than a single agent, so that antibodies to the virus would not be able to contain all the variants present in his blood. Because of this unique characteristic of the H strain virus, it became the standard challenge dose for most subsequent studies of prototype hepatitis C vaccines and has been used to develop tissue culture models. "All this was possible because of Hutchinson’s interest in science and his willingness to provide blood samples and to allow investigators to distribute them to laboratories throughout the world. Hutchinson’s name is known throughout the global hepatitis community and we are all indebted to him," Alter said.
Hutchinson says he’s pleased that his blood could be useful, even if his involvement with clinical research was mostly an accident. "If my blood saves even one life, that’s good. If it saves more, so much the better."
The NIH researchers who gathered to meet Hutchinson assured him of how much they, and other hepatitis patients, have learned from him. Alter told Hutchinson that researchers are working with purified antibodies isolated from his blood to measure their ability to neutralize the virus and to see if these antibodies could be useful as a prototype therapeutic agent. Farci told Hutchinson how her ability to tell other hepatitis patients that someone has lived with the virus for 30 years to reach age 90 encourages them in their struggles with the condition.
Hutchinson credits his long life to keeping active walking, hiking, and clearing trails, especially for the first 20 years of his retirement. He is father to four adult children and grandfather to more than 20 grandchildren, although he says he "hasn’t counted lately." When asked what he’s learned from all of his unique life experiences, he said it was that "all people, no matter where they are from, should be treated with respect. No one is better than their neighbor." Hutchinson demonstrates that same altruism and humility as a donor. "I never imagined that this would come from all those quiet little sessions I’ve had here," he said. "I’ve always been treated well here."
The group presented Hutchinson with a framed aerial photo of NIH for his 30 years of participation in clinical research, as well as a letter that they all signed expressing their deep gratitude for "his selfless and unwavering willingness to be a research subject. His efforts have helped to diminish the risks and chronic consequences of this highly prevalent infection and to vastly improve the safety of the blood supply."
Back to Top
Surgeon General visits Clinical Center
 |
|
Rear Admiral and Acting Surgeon General Dr. Kenneth Moritsugu meets CC patient Brenda Bain, whose blood glucose levels were managed by the BGMS during her stay. "My time here has been wonderful. They’ve treated me very well," Bain said, adding, "I’m happy to know I’m not alone in taking care of my diabetes."
|
During a July 20 visit to the Clinical Center, Rear Admiral and Acting Surgeon General Dr. Kenneth Moritsugu learned about the new pilot Blood Glucose Management Service (BGMS), a collaborative effort for managing insulin orders for CC inpatients with hyperglycemia.
Seven years ago, Moritsugu was diagnosed with latent autoimmune diabetes of adults, a less common form of type 1 diabetes. He wears an insulin pump to manage his condition and is especially interested when visiting NIH to learn about initiatives involving patients with diabetes. Always reminding staff of their work’s impact on the health of the country, especially U.S. residents with diabetes, Moritsugu showed the BGMS team his pump, saying, "This isn’t a pager that I’m wearing!"
Medications and other conditions, such as stress, can bring on high blood glucose levels similar to the disease. BGMS treats inpatients with hyperglycemia, or high blood glucose, at the request of their CC care team. The group estimates that at any given time, about 10-20 percent of CC patients have hyperglycemia. The BGMS’ sole function is to focus on this blood glucose management.
A multidisciplinary team of CC staff, including physicians, nurses, pharmacists, dietitians, diabetes educators, CRIS developers, and endocrine fellows, developed the BGMS, noting studies that are increasingly showing that intensive blood glucose control is important for patients’ prognosis in the hospital. The higher the blood glucose, the higher the mortality rates from the many problems that could develop, including decreased cellular, vascular, and renal health, according to NIDDK Diabetes Branch Chief Dr. David Harlan. Managing blood glucose can help patients with glycemic challenges achieve the same outcomes as patients without hyperglycemia.
 |
|
NIDDK Diabetes Branch Chief Dr. David Harlan (standing) gives an introduction to the Blood Glucose Management Service to Rear Admiral and Acting Surgeon General Dr. Kenneth Moritsugu during the group’s daily blood glucose rounds. Moritsugu’s insulin pump can be seen on his left hip.
|
"We believe such a system can also serve an extremely important role for our endocrine training program and as a platform for important research questions," said Harlan. "We don’t want patients’ glucose levels to ever negatively affect the outcome of their treatment in the hospital." Within 24 hours of an inpatient referral to the BGMS, endocrine fellows are responsible for gathering the appropriate initial clinical intake information, discussing plans with attending physicians, and writing insulin orders.
Each CC unit participating in the pilot program—currently 1 NW, 3 NE, 3 NW, 5 SE, 5 SW, 5 NW, and 7 SW—has a BGMS ambassador who checks on the unit’s patients. The ambassadors track dosage issues that result in low or high blood glucose and discuss them at the group’s daily rounds. Team interdisciplinary notes are recorded daily in CRIS and insulin orders are modified as necessary. A BGMS team member is always on call, and one pager is shared within the group to make it easy for nursing staff to reach the team with questions. It has not yet been decided when the service will be offered CC-wide, and the pilot program’s current capacity is about 15 patients per day.
The BGMS welcomes referrals to their service for inpatients with above normal blood glucose, and staff who are interested in learning more about managing hyperglycemia are welcome to attend rounds with the group.
Back to Top
DTM gives four summer students first job
 |
|
(from left): Keaira Dowdy, Bianca Powell, Ashley Belcher, and Avis Brown look through the photo albums with more than 50 years of CC and DTM history that the summer students assembled during their time here, as Avis Brown points out prominent public figures in the images. Not pictured: DTM summer student Jordan Jett.
|
Avis Brown, supervisory program support specialist in the CC Department of Transfusion Medicine, went the extra mile this summer to provide early lessons about professionalism for four students. On her own initiative, Brown brought four high school students—Ashley Belcher, 17; Keaira Dowdy, 15; Jordan Jett, 15; and Bianca Powell, 18—to work as summer students in the department.
"I’m extraordinarily grateful to Avis for making this happen," DTM Chief Dr. Harvey Klein said. "Once again, the Clinical Center is contributing to helping young people get a start in their careers and to learn the basics of what it takes to have a job. Even if they’re not working with world-class scientists in the future, they now know how to interact and approach people professionally. I’m so pleased to have them here helping out, and I appreciate their enthusiasm and willingness to do whatever needs to be done."
At the start of the summer, Brown invited the four students and their parents to attend a special orientation day to present information on how to manage your paycheck, professional attire and behavior, and team work. On their first day, she sent the students on errands all over the CC and campus to help them learn their way around. They weren’t allowed to ask DTM staff for directions and had to collect signatures from NIH staff at each location, so the assignment became a scavenger hunt.
The students also interviewed a few of the more than 125 DTM employees about their jobs and themselves and summarized their findings in a regular newsletter so that they would learn about career development opportunities. Staff soon discovered an excellent side effect of the newsletter assignment: They learned things about their colleagues that they might never have asked otherwise, such as what superhero or cartoon character they would like to be, whether they would ever wear their hair in a Mohawk, and whether they sing in the shower. The group also asked Klein those types of questions, who noted that although he’d appeared on the "Today Show" and done a lot of other interviews, he’d never had one by four high school students. "I’d almost forgotten how much fun it is to have kids here, to see them grow, and see how appreciative they are of opportunities."
DTM had plenty of work to keep the students busy. Brown coordinated staff requests for help from the students. They archived and filed about 50 years of photos of blood bank donors into albums. Brown pointed out prominent researchers, politicians, and other public figures who played a part in CC and DTM history. They also color-coded and filed blood donor files and stuck labels on vials used in blood donations and the cards sent to donors.
"It was very helpful for us to have the students’ assistance," said DTM nurse Rosemary Werden, who works with healthy donors collecting white blood cells for research. "Those routine jobs can be very time-consuming, and the summer students help us catch up on administrative projects. Their energy and enthusiasm is also contagious."
All the students said they would love to return next summer and the experience whet their interest in federal careers. The students absorbed Brown’s mentoring and received rave reviews from staff. "They are all so polite and respectful, as well as a boatload of energy," Brown said. "It’s kept me busy keeping them busy." DTM Chief Operations Officer Betsy Jett said that she was "very impressed by how Brown handled the students. "I think she’s found her real calling in life. The students have been very helpful and it is so refreshing to have young people working here again."
Back to Top
Simulation classroom provides a safe space for staff to push skills
 |
|
Rose Simpson (left) and Wendy Moore, both clinical research nurses on 3NE, participate in a live-action scenario in the clinical simulation classroom.
|
"Help, help! She’s been agitated all day and now I don’t think she’s breathing!"
Although a Clinical Center staff member is speaking these words, she is playing the role of a bedside nurse in a "live action" scenario in the Critical Care Medicine Department’s Clinical Simulation Classroom on the fourth floor of the Hatfield Building. The female patient is a computer-operated mannequin. She’s a resource available to CC and other NIH staff looking to polish their technical skills for unfamiliar or uncomfortable clinical procedures, practice critical thinking in an emergency, and build team cohesion.
Simulation is being used at many hospitals and medical schools as a major teaching device for students, residents, and full-time staff. Many universities have large complexes with dozens of simulators so that staff can be trained in a variety of scenarios on a regular basis.
CCMD launched the service with the purchase of a Laerdal SimMan and audio-visual package in 2003 to teach critical care medicine fellows, and eventually post-graduate nurses and respiratory therapists, how to respond in less frequently encountered emergency events. The high-fidelity, full-body mannequin, which is more advanced than the basic models used for CPR training, can simulate a number of emergency events, such as a blocked airway, cardiac arrest, or internal bleeding after surgery. The mannequins can also be used to practice chest tube insertion, tracheostomies, and periocardiocentesis. The mannequin—called William Simman for a male patient or Wilma Simman for a female patient—can also be shocked and intubated and can produce a variety of life-like heart and breath sounds.
 |
|
Dr. Amy Agrawal programs the scenario into a computer, which controls the mannequin’s life-like sounds, while Jill Sanko monitors the video feed.
|
Training to lead effective simulation education courses requires intensive orientation. National conferences and courses train simulator educators in how to assess and improve efficacy. CCMD's Dr. Amy Guillet Agrawal and Jill Sanko, certified registered nurse practitioner with NHLBI, both attended a week-long workshop at Harvard University’s Center for Medical Simulation and began regular training sessions at the CC in January 2005. CCMD nurse Nancy Muldoon recently joined the staff and completed the same training workshop. Agrawal and Sanko now lead between five and ten training sessions in the room each week. CC units using the simulation service include 3NE, 3NW, 3SW, respiratory therapy, and the oncology day hospital.
Most classroom simulations are "live action," where participants are thrown into a simulated clinical scenario and the action is allowed to unfold as in a real crisis. This puts participants under mild stress, which Agrawal and Sanko say helps them teach rapid critical thinking and decision-making skills. It also helps participants retain the information they are learning. When the training scenario ends, CCMD staff lead a debriefing. The participants and instructors may watch themselves on video tape, reflect on their performance, and review the learning objectives. Usually only two or three people participate at one time to make sure that the situation forces everyone to get involved. Agrawal says the classroom is good for simulating a crisis and observing group dynamics in an emergency. Participants learn clean and effective communication, how to prioritize and delegate tasks to reduce confusion, and choreograph a successful response.
The classroom is also used for "static" scenarios, where participants and an instructor talk and work through a clinical problem with multiple interruptions for teaching purposes.
Agrawal and Sanko create a non-threatening environment by keeping participants’ scores and videos confidential. Just like Las Vegas, what happens in the simulation classroom stays in the classroom—information on a specific individual’s performance is not shared with supervisors. But they purposely raise participants’ anxiety levels. "You never forget about a mistake if you make one on a real patient. We try to simulate that experience here, without the possibility of anyone getting hurt," Agrawal said. "Until you live through the actual thing, you don’t know if you’ll remember the things you read in a book." ICU nurse Heather Rhine said that working through the effects of stress created in the simulation classroom increased her confidence and preparation for real-life emergency situations. After practicing resuscitation skills in a life-threatening blocked airway scenario in the classroom, she later accurately assessed and corrected a patient’s condition, thus helping to save a life.
Kate Castro, an oncology clinical nurse specialist, approached Agrawal and Sanko when 3NE oncology nurses identified a need for practice with chest tubes, a low-volume but high-risk technique. Oncology nurses are more frequently caring for patients with chest tubes. The device drains fluid and air from around the lungs to relieve patient symptoms.
 |
|
The Clinical Simulation Service team: Dr. Amy Guillet Agrawal, Nancy Muldoon, and Jill Sanko.
|
After Castro, Agrawal, and Sanko developed a chest tube scenario in November, all 40 3NE nurses in January began training two at a time in the classroom. The experience has been very positive for the staff, according to Castro, even though it is the first time many of them have used the simulation room and they may be apprehensive or anxious. Still, most people can suspend their disbelief enough to get comfortable with the mannequin and learn some valuable lessons. Castro found the service so valuable that she will incorporate simulation work into the CC’s oncology nurse internship program. "You learn well because you’re pushed by the heightened sense of awareness that the simulator brings," Castro said. Betty Maestri, one of the first clinical research nurses on 3NE to visit the classroom, said the experience made her feel "more grounded, confident, and able to solve problems" when she encounters a patient with a chest tube. On evaluation forms, more than 94 percent of respondents say the classroom training was worth their time, and 96 percent say simulation training should be mandatory.
Castro said the simulation service staff "deserve a great deal of credit for making people feel comfortable. They tell you not to worry about making mistakes, because you will make mistakes, but this is the place to make them." Her team’s experience with the service has "raised the bar on standards for high-risk situations," prompted a reorganization of their emergency kits for chest tubes, and increased real-time discussions about managing patients with chest tubes. "I know we’ve improved our patient care by participating," Castro said.
Although it would be difficult to pinpoint medical simulation training as the reason for a reduction in medical errors, there are clear anecdotal connections. Sanko receives calls from participants who experienced the same scenario in clinical work that they practiced a few weeks ago in the classroom. "They say the ability to rehearse what they would do and learn from any mistakes really makes an impact."
Agrawal and Sanko are completing the first year of a program to assess ICU fellows’ skill retention through the simulator. All ICU fellows must complete six emergency scenarios when they begin working at the CC. Their reactions in the scenarios are videotaped and scored by Agrawal, Sanko, and a third instructor, depending on the topic. ICU fellows repeat the scenarios at the end of a full year of clinical training to see if their scores improved. Agrawal and Sanko this summer also published a chapter on how to begin a medical simulation program with minimal resources and cost in the book, Clinical Simulation: Operations, Engineering and Management.
The airline industry, which relies extensively on simulators to train pilots, was a model for the methods that health professionals use to debrief medical simulation experiences. The Institute of Medicine, the Agency for Healthcare Research and Quality and the Institute for Healthcare Improvement now endorse simulation. Papers on its use to train physicians and nurses are emerging in the medical and nursing literature. In addition, the Accreditation Council for Graduate Medical Education includes medical simulation in its "training toolbox" as a means of verifying competencies among residents and fellows.
The Clinical Simulation Service welcomes anyone with a training need to contact them at 301-496-9320. Their current inventory includes multiple scenarios for physicians, nurses, and respiratory therapists, and they are happy to work with clinical educators to develop more. Castro encourages other units to collaborate with the simulation service. "They pour their whole heart and soul into making your team’s experience as life-like as possible. It’s an incredible resource, and we need to be creative in discovering ways to use it more."
Back to Top
Housekeeping, Fabric Care Department's customer service keeps CC clean
 |
|
(from left) Errol Smith, Frank Greenwell, Raymond Patterson, and Chauncey Buford load bundles of clean laundry onto carts for transport to patient units.
|
It goes without saying that hospitals need to be clean to provide sanitary conditions for patient care. But the Clinical Center’s Housekeeping and Fabric Care Department (HFCD) takes their mandate to the next level.
HFCD’s 55 federal and 128 contract employees are responsible for providing housekeeping services for patient, public, and laboratory areas; testing new cleaning equipment and supplies; assuring that sanitary conditions are met; providing linens for patient care, research, and service areas; repairing and altering linens and garments; fabricating new linen items in special circumstances; and ensuring compliance with established laundry standards.
That may seem straightforward until you imagine what Building 10 would be like if the housekeeping staff, who are essential employees, suddenly weren’t there. Joe Cowling, housekeeping supervisor for waste and recycling, estimates that if his team were absent, by about 2 p.m. the entire north B2 hallway would be lined end-to-end with filled blue trash carts. "We play a very important role in fulfilling the CC’s mission," HFCD Chief Rob Mekelburg said, noting that it is a team effort provided by a group of dedicated employees.
 |
|
Juanita Coleman, quality assurance inspector, checks an empty patient room on 3SE to see if it received a thorough cleaning.
|
Most HFCD teams divide their staffs into shifts to provide coverage in responding to CC clinical staff requests from 6:30 a.m. until midnight. Chauncey Buford, laundry manager for all services within Building 10, the Children’s Inn, the Safra Family Lodge, the firehouse, as well as lab coats on campus, said his team’s goal is to respond to any unscheduled requests within 10 minutes. The connection between emergency linen requests and the CC mission is very clear, such as providing a blanket for a patient who is cold while undergoing a procedure, or replacing bedding.
CC patients receive not only the best possible care, but also the best possible environment for receiving that care. According to Juanita Coleman, quality assurance inspector, although most hospitals would clean patient areas primarily after discharge, the CC cleans everything thoroughly every day. HFCD staff also communicate frequently with nurses on their assigned units to clean areas as needed. Staff learn from their initial week of training that they will be held accountable for customer service skills and rigorous cleaning and safety standards. Coleman walks through all public and patient-care areas daily to make sure they are clean enough and comply with safety rules, such as stocking enough supplies like gloves and goggles, not mixing chemicals, and storing locked carts in locked closets. Coleman, who began her CC career as a housekeeping aide before becoming a team leader, supervisor, and now quality inspector, said the department "is a good place for people to develop themselves."
 |
|
Supply technician Troy Cotton orders and stocks the multiple cleaning supplies the department uses.
|
High standards are required of the contractors and vendors who supply the CC with their labor and products. NIH is also a member of the National Fabric Care Institute, which can monitor linen thread counts and the chemicals used on fabrics to ensure an appropriate lifespan.
Clean and soiled laundry can not occupy the same truck, so the department runs a tightly orchestrated schedule. Soiled linens are picked up at 5 a.m., clean laundry comes in on a truck between 6 and 7:30 a.m., and a second batch of soiled linens are loaded onto the truck after the clean laundry is unloaded. Laundry bundles leaving and arriving are weighed. Soiled laundry is heavier than clean, but there shouldn't be a significant discrepancy.
The seven laundry services staff members function as a team to give their customers the type of linens they need, which can vary widely. For example, pediatric units like to cheer up their young patients with brightly colored and patterned pajamas, gowns, and sheets, which would not work in an operating room. All OR linens are green to separate them from the rest of the CC’s linen, which is white and does not require the same special cleaning procedures as items worn in surgical areas. When investigators launch new protocols, they contact Buford to discuss their linen needs. For example, the opening of the obesity protocols for the Metabolic Clinical Research Unit prompted Buford to order fitted, knitted sheets that will fit on the larger beds.
 |
|
Brenda Cotton distributes clean mops into buckets for distribution throughout the CRC, which uses about 36 mop buckets daily.
|
Then there’s the issue of supplying housekeeping closets and carts with the supplies necessary for cleaners on the units to do their jobs. Supply technician Troy Cotton orders and stocks the multiple cleaning supplies the department uses, such as dust cloths, spray cleaners, bed disinfectants, and hand soaps. Other staff members, including Ramon "Poncho" Rodriguez, group leader for housekeeping, make daily rounds with heavy carts to fill areas with supplies, swap dirty mop tops with clean ones to Velcro on the mop handles, and empty trash bins. The connection to the CC mission Rodriguez’s job might seem remote to some, but he’s clear on how it helps patients, noting, "The mops are needed to help keep the patient care areas clean." And the delivery roles keep HFCD staff on their toes, literally. Rodriguez said since he began pushing carts he lost 27 pounds.
 |
|
Joe Cowling, housekeeping supervisor for waste and recycling, pushes a blue trash bin into the roll-through cart wash on the B2 loading dock.
|
Even the trash bins themselves are regularly cleaned in roll-through washing stations that resemble miniature car washes on the B2 loading dock. Reggie Britton, one of the housekeeping aides responsible for cleaning-related activities on that level, washes about 40 to 50 of the CC’s trash bins each day.
So the next time you reach for the soap dispenser to wash your hands, put out your trash and recycling, or drop off your lab coat or scrubs to be laundered, remember the often unseen HFCD staff who make sure the CC is not only the country’s premier research hospital, but also as clean as possible.
Back to Top
Barbara Fabian Baird, pioneer CC HIV/AIDS nurse researcher, dies
 |
|
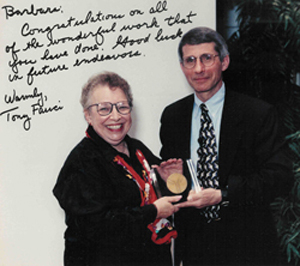
Barbara Baird with NIAID Director Dr. Anthony Fauci at the 1999 NIAID Director’s Annual Report and Awards Ceremony. She received the award "for outstanding contributions to the intramural HIV clinical research program" of the Nursing Study Coordinator Group (DIR). The inscription on the photo reads: "Barbara: Congratulations on all of the wonderful work that you have done. Good luck in future endeavors. Warmly, Tony Fauci."
|
Barbara Fabian Baird, a Clinical Center nurse who was among the first to treat patients with HIV/AIDS, died August 7 at age 69 after hospitalization for a brief illness.
Baird supported and conducted ground-breaking research that eventually led to the identification and treatment of HIV/AIDS. At a time when nurse researchers were uncommon, Barbara cared for terminally ill patients, collected and stored biologic specimens, gathered and processed data, co-authored scientific papers, and traveled around the country teaching other nurses how to care for AIDS patients. She was a pioneer in developing the role of study coordinator and case manager.
Originally from Charleroi, Pa., Baird later settled in the Washington, D.C., area to raise her family. She graduated from George Mason University with a Bachelor of Science in nursing in 1979 and a Master of Arts in communication from the University of Oklahoma in 1994. She came to NIH in March 1981 after hearing from a patient how impressed he was with the care and research conducted at the CC. Baird started as a staff nurse on OP11 East, the unit for patients with immune disorders and infectious diseases.
In NIH’s oral history project, "In Their Own Words: NIH Researchers Recall the Early Days of AIDS," Baird described the challenges of treating patients with unexplained immune dysfunction when they started to appear in the winter of 1981, including helping physicians develop specific infectious disease guidelines, collecting information without knowing if it would later indicate something meaningful, and managing the "overwhelming" fear of some staff without stigmatizing or isolating patients any more than they already were. According to Baird, she "just fell into" her work with HIV/AIDS, saying it "offered an opportunity at a particular time. I was right there, and I wanted to take advantage of the opportunity to learn about a new disease."
Baird described encountering suspicion and stigma for her vocation, "like I wore a big letter ‘A’." She remembered the response she received when she described her work with AIDS research to a neighbor who welcomed her after a move. "I thought she was going to kick me out of the neighborhood. She said, ‘I’m surprised you even tell anybody about it.’ About the same time, or maybe shortly before that, my dentist and my doctor wrote on my chart, ‘Works with AIDS patients.’"
Despite her precautions, Baird experienced several needle sticks, including one from the first AIDS patient at NIH. "I was used as the index case to show that hepatitis is more infectious than AIDS," Baird said in 1993, noting that despite a subclinical hepatitis case and elevated liver enzymes, her HIV status remained negative. "None of those needle sticks would happen today because of the safety measure that have been instituted. All of the precautions I was using were adapted as the protocol for these patients with AIDS. I did not know that I was protecting myself against HIV because we did not know then that AIDS was caused by a virus."
Bill Barrick, former head nurse of the HIV clinic, recalls that Baird was a pioneer in the role of nurses as study coordinators and data managers and showed how traditional nursing knowledge and aptitude were essential to developing a professional role for nurses in clinical research.
She always approached her work by putting the needs of others before her own. Dr. Henry Masur, chief of the CC Critical Care Medicine Department and current president of Infectious Diseases Society of America, called Baird "a positive part of NIH history" who "took many young men under her wing in an era when few others would." OP12 program assistant Carolyn Foulks said Baird was "so on point with making sure her patients were taken care of" and she "loved and respected the people who came to OP11, people who perhaps had been mistreated before they came to NIH. She will be missed by everyone who knew her and remembered as a great icon in the medical field: a trooper and a strong person, one of the best." Senora Mitchell, an administrative assistant in the HIV clinic on OP8, remembers Baird as an avid tap dancer and a fanstastic person who could always make others laugh. "She loved her patients and she gave them hugs and kisses when no one else wanted to touch them," Mitchell said. Sandy Montgomery-Aker, NCI, called Baird "the best friend that anyone could have. She was able to heal many troubled souls with her words and wonderful smile."
Baird is survived by her brother, Stephen Fabian; her three sons, Bruce Baird, Bob Baird, and Bryan Baird; and her twelve grandchildren.
A complete transcript of the oral history interview conducted in 1993 with Baird about her work at NIH is available at http://history.nih.gov/NIHInOwnWords/docs/baird_01.html.
Back to Top
CCMD mathematical statistician Steven Banks remembered
 |
|
Steven Banks, CCMD mathematical statistician
|
Steven M. Banks, mathematical statistician in the Clinical Center's Critical Care Medicine Department, died suddenly of a heart attack August 10 in Temple Terrace, Fla. He was 51.
A nationally recognized expert in the field of mental heath statistics, Banks received his doctorate in mathematics from the State University of New York at Albany in 1987. He trained with NIAID’s legendary Dr. David Alling, a pioneer in the application of statistical methods to biomedical research who helped investigators define the population sample needed to show efficacy of a particular therapeutic agent, develop clinical protocols, randomize the drug treatment, and analyze statistical data.
Banks was also the chief mathematician of the Bristol Observatory and founding partner of Paradigm Associates. A native of Gaithersburg, Banks held research associate professorships in the Department of Psychiatry at the University of Massachusetts and the Louis de la Parte Mental Health Institute at the University of South Florida.
Banks wrote hundreds of articles for professional journals and held a U.S. patent for a method of estimating population size. He received the NIAID Director’s Award in 1990 and the Guttmacher Award for the publication Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence in 2002.
Banks, a cancer survivor of more than fifteen years, loved thinking about problems and worked tirelessly with scientists in many different fields to solve them. According to Dr. Charles Natanson, an investigator in CCMD, Banks was also an amazing teacher. "He required no slides or other audiovisual aid, just some chalk and he could absolutely enthrall an audience speaking about statistics—really!"
In his eulogy, Natanson remembered Banks as "a defender of human life, courageous warrior for principle, and unwavering seeker of truth." For example, when HA-1A was approved for the treatment of sepsis in Europe, Asia, and Australia, the FDA was in the process of reviewing the data for U.S. licensing. Banks helped design an animal study to evaluate HA-1A’s efficacy and found that the agent increased mortality in the septic animals.
Banks and Natanson met with the company at FDA. A bus pulled up and multiple famous scientists and statisticians showed up—all in suits, ties, and high heels. Banks, in jeans with shoulder-length hair, "held the day in a David-and-Goliath-like showdown" with the company statisticians to show it was a statistically significant finding, Natanson recalled. "In his quiet, steadfast way, Steve engaged in the verbal sword fight for more than two hours, as he dispassionately and with great clarity fended off each attempt to discredit the study. The FDA required another human sepsis trial of HA-1A, which confirmed the harm we found in animals, and it was learned the initial work suggesting HA-1A worked in human sepsis was fraudulent. The drug was removed from human use worldwide. We learned from this experience that as U.S. government employees we can help protect the public because we were in a unique position, not beholden to anyone," Natanson said. "Thus began our almost two-decade odyssey of chasing windmills. In our case, the windmills were potentially harming patients and research subjects. Steve toppled them to help save lives and to make the world a better place."
Banks is survived by his wife, Cheryl McCathran, whom he married on December 30, 1978, and who currently resides in Berne, N.Y.; his parents, Joseph and Charlotte Banks of Rockville; sisters Amy (Stuart) McIntyre of Germantown; Nancy (Joseph) Cauley of Columbia; and Beth (Terry) Colvin of Windermere, Fla.; brother Jeffery; (Barbara) Banks of Rockville; and several nieces and nephews.
Contributions may be made to the Steven M. Banks Memorial Fund in care of TD Bank North, 343 Delaware Ave. Delmar, N.Y., 12054, in lieu of flowers.
Back to Top
New recycling containers gleam in Clinical Center spaces
 |
|
Two new recycling containers next to the large, circular metal trash container that inspired their look. The trio of containers will often be grouped close together.
|
The high-traffic public spaces in the Clinical Center began to shine a little brighter at the start of September with the arrival of 50 new metal recycling containers.
Designed to match the large, circular metal trash containers and to replace some of the older, square red recycling bins, the new containers also feature inscriptions in English and Spanish describing their contents: "Plastic, metal, glass" or "Mixed paper."
Having two recycling containers—instead of three or four as is currently the case in some areas—reflects the industry standard of more commingling of varied materials, as occurs for most home recycling.
 |
|
Two new recycling containers in front of the old recycling bins.
|
It is also hoped that the new containers, designed especially for the CC by Medical Arts and the CC art committee, will also contribute to an aesthetically appealing and serene environment in public areas.
Back to Top
News Briefs
September is national sickle cell awareness month
The Sickle Cell Disease Association of America’s 35th annual conference, which is co-sponsored by NIH and NHLBI, will be held Sept. 17-22 at the Washington Hilton. More information and online registration are available at www.sicklecelldisease.org/info/2006_convention.phtml. The Stomp Out Sickle Cell (SOS) Walk to raise community awareness of the disease will be held on Sept. 22 from 9 a.m. to noon. The walk will begin in front of Howard University Hospital at 8:30 a.m. See www.SOSwalk.org to register or call 202-865-4443.
Transfusion Medicine hosts symposium
The Clinical Center’s Department of Transfusion Medicine, together with the American Red Cross, will host the 26th annual symposium on immunohematology and blood transfusion on Sept. 20 in Masur Auditorium. CC staff participating in the program include: Drs. Harvey Alter, Barbara Bryant, Cathy Cantilena, Harvey Klein, Susan Leitman, David Stroncek, and Sumithira Vasu. For more information, see www.cc.nih.gov/dtm.
NICHD hosts world’s second pheochromocytoma conference
Medical professionals, patients, and families are invited to attend NICHD’s second annual conference on pheochromocytoma, a rare form of cancer that often begins in the adrenal glands, on Sept. 28 and 29 at Bethesda’s Doubletree Hotel. CC staff Dr. Jacques Bolle, clinical thanatologist, and Dr. Brad Wood, chief of interventional radiology research and acting co-chief of the Diagnostic Radiology Department, together with other NIH researchers and international specialists, will give presentations. For program information or to register, see www.pheochromocytoma2007.nih.gov/cns/index.html.
Back to Top
New clinical research protocols
The following new clinical research protocols were approved in July:
A Double-Blind Randomized Phase 2.5 Trial of ONY-P1 Vaccine Versus Placebo in Men with D0 Prostate Cancer Following Limited Androgen Ablation, 07-C-0188, James L. Gulley, MD, NCI
Phase I/II Trial of Vandetanib (ZD6474, ZACTIMA) in Children and Adolescents with Hereditary Medullary Thyroid Carcinoma, 07-C-0189, Frank M. Balis, MD, NCI
Pilot Trial of Targeted Immune-Depleting Chemotherapy and Reduced-Intensity Allogeneic Hematopoietic Stem Cell Transplantation Using HLA-Matched Unrelated Donors and Utilizing Two Graft-Versus-Host Disease Prophylaxis Regimens for the Treatment of Leukemia, 07-C-0195, Michael R. Bishop, MD, NCI
Phase 1, Multicenter, Dose-Escalation Study of CAT-8015 in Patients with Relapsed or Refractory Non-Hodgkin’s Lymphoma (NHL), 07-C-0200, Robert J. Kreitman, MD, NCI
Detection and Treatment of Endocrine Abnormalities in Childhood Cancer Survivors, 07-CH-0192, Maya B. Lodish, MD, NICHD
Use of GnRH Antagonist to Preserve Ovarian Function in Women Undergoing Chemotherapy, 07-CH-0193, Alicia Y. Armstrong, MD, NICHD
Genes Causing Congenital Ebstein’s Anomaly, 07-H-0186, Cecilia W. Lo, PhD, NHLBI
Niacin Therapy to Improve Endothelial Function in Sickle Cell Disease, 07-H-0196, Gregory J. Kato, MD, NHLBI
A Phase One Treatment Trial of the Circadian Sleep Disturbance in Smith-Magenis Syndrome (SMS), 07-HG-0076, Ann C. M. Smith, NHGRI
Brain Connectivity and Sensorimotor Integration During Single/Dual Motor Tasks, 07-N-0187, Mark Hallett, MD, NINDS
Neurobiological Studies of Psychogenic Movement Disorders and Non-Epileptic Seizures, 07-N-0190, Valerie Voon, MD, NINDS
Role of the Cortical Medial Frontal Areas in Blepharospasm, 07-N-0191, Mark Hallett, MD, NINDS
Back to Top
Research volunteers needed for studies
Neck pain study
Volunteers with or without neck pain ages 18 to 65 needed to participate in a three-month natural history study (02-CC-0245) involving four one-hour visits. Contact neckpainstudy@gmail.com, 301-496-4733.
Back to Top
Medicine for the Public series begins Oct. 2
The Clinical Center will present its annual series of lectures on important health topics on four Tuesdays in October. The lectures are free and open to the public. All begin at 7 p.m. in Masur Auditorium.
Tuesday, October 2, 2007
"Alcohol Use Disorders: Old Insights, New Treatments"
Markus Heilig, M.D., Ph.D., Clinical Director, NIAAA
Seventeen million people in the U.S.—about 1 in every 12 adults—abuse alcohol or are alcohol dependent. Alcoholism is a disease, and research shows that the risk for developing alcoholism runs in families. The genes a person inherits partially explain this pattern, but lifestyle is also a factor. The craving that an alcoholic feels for alcohol can be as strong as the need for food or water. Despite serious family, health, or legal problems, an alcoholic will continue to drink. This lecture will cover alcoholism, its symptoms, and the latest research on the disease.
Tuesday, October 9, 2007
"The Prevention of Cervical Cancer by Vaccination and Other Means"
Douglas Lowy, M.D., Chief, Laboratory of Cellular Oncology, Center for Cancer Research, NCI
Cervical cancer is the second most common cause of death from cancer among women worldwide. Although detection by Pap smear has made a substantial impact on the incidence of this disease, FDA’s approval of a new human papillomavirus vaccine (HPV) in June 2006 represents an enormous advance for public health. While most HPV infections do not lead to cancer, virtually all cervical cancer cases are caused by HPV infection, and two of the HPV types targeted by the vaccine cause about 70 percent of cervical cancer cases worldwide. This lecture will include an overview of cervical cancer prevention strategies, including use of the HPV vaccine and Pap smear.
Tuesday, October 16, 2007
"Childhood Blindness to Age-related Macular Degeneration: Genes, Eye Disease, and Prospects for Therapy"
Paul Sieving, M.D., Ph.D., Director, NEI
Nearly 450 genes lead to vision loss. Gene transfer and cell transplantation are among the new treatments that can benefit people with eye disease. This lecture will describe the range of eye-related genetic diseases and will explore cutting-edge eye disease treatments.
Tuesday, October 30, 2007
"Good Pain, Bad Pain: New Advances in Pain Mechanisms and Treatments"
Michael J. Iadarola, Ph.D., Chief, Neurobiology and Pain Therapeutics Section, Laboratory of Sensory Biology, NIDCR
There are about 500,000 cancer deaths a year. Of those, about 50,000 people die without receiving adequate relief from the excruciating pain caused by the disease. This lecture will cover the development of a novel pain therapy that selectively kills pain-causing cells while leaving other sensory neurons intact. This results in permanent pain relief without the debilitating side effects of traditional pain-killing medications. Experiments in the laboratory and in animals have been successful, and testing in humans will begin soon. The speaker will also discuss the basis of pain and the history of pain diagnosis and treatment.
For more information, call CC Communications, 301-496-2563 or see http://clinicalcenter.nih.gov/about/news/mfp.shtml.
Back to Top
Upcoming Events
September 5, 2007
T-2 Weighted Imaging of the Heart:From Spin-Physics to Physiological Validations
Anthony Aletras, Ph.D.
Staff Scientist, Cell Biology and Physiology Center, NHLBI
The Ischemic Area at Risk: Implications for Clinical Trials of Acute Myocardial Infarction
Andrew Arai, M.D.
Senior Investigator, Cell Biology and Physiology Center, NHLBI
September 12, 2007
Great Teachers
Contemporary Clinical Medicine: Great Teachers
The Vocation of Medicine: Lessons from Real and Imagined Doctors
Paul Plotz, M.D.,
Chief, Arthritis and Rheumatism Branch, NIAMS
Lecture will be videocast, http://videocast.nih.gov
September 19, 2007
Closing the Gap Between Imaging and Therapy in the Operating Room of the Future
Brad Wood, M.D.,
Acting Co-Chief, Diagnostic Radiology Department, and Chief, Interventional Radiology Research Laboratory, CC
Non-Invasive, Image-Guided Drug and Gene Delivery Using Focused Ultrasound
Victor Frenkel, Ph.D.
Head, Therapeutic Ultrasound Research, Molecular Imaging Laboratory, Diagnostic Radiology Department, CC
September 26, 2007
No Grand Rounds.
Other events: NIH Research Festival
For more information, see http://researchfestival.nih.gov
Back to Top
Clinical Center News, National
Institutes of Health, Building 10, 10 Center Drive, Room 12C440, Bethesda, MD 20892-1504. Tel: 301-496-6787.
Fax: 301-402-2984. Published monthly for CC employees
by the Office of Communications, Patient Recruitment, and Public Liaison. News, article ideas,
calendar events, letters, and photographs are welcome.
Back to Top
|
|


 The information on this page is archived and provided for reference purposes only.
The information on this page is archived and provided for reference purposes only.