Winter 2016
IN THIS ISSUE:
![]()
- Gallin appointed to new leadership position
- The sweet smell of gingerbread houses fill the atrium
- Clinical Center employee chases dream, changes career
- Dr. Paul Farmer, founder of Partners in Health, speaks at NIH on global health equity, visits pediatric patient from Peru
- Annual government survey shows staff satisfaction with work, desire for additional resources and more leadership support
- Five NIH grants awarded for collaborative research in the Clinical Center, across the U.S.
- Hooray for Caregiver's Day! NIH celebrates people who provide patient support
- Experts from NIH and the Middle East cure patient with rare tumor
- Travel Office connects patients with cures
- Dr. Nicholas Patronas, CC neuroradiology section chief, retires
- Five recent graduates of nursing school complete Clinical Research Nursing Residency Program
- Former NIH trainee returns to lecture on leading cause of pediatric acquired heart disease
- UNC professor presents Astute Clinician Lecture on autoimmune swelling of blood vessels
- Over $2,500 raised for charity at CFC bake sale
- Hurry! CFC extended to Dec. 31, 2016
- A celebration of Nurse Practitioners, who are a crucial part of the patient care team
- California radiogenomic expert presented annual Doppman Memorial Lecture
- 9/11 survivor discusses challenges, inclusion
- Study participants needed for a trial on the health of the heart and blood vessels and a trial seeking to help prediabetic overweight and obese individuals
- Upcoming Events
Print this Issue ![]() (688 KB)
(688 KB)
ABOUT CC NEWS:
![]()
Published monthly by the Office of Communications and Media Relations. News, article ideas, calendar events, letters, and photographs are welcome. Submissions may be edited.
Clinical Center News
National Institutes of Health
Building 10, 10 Center Drive
Room 6-2551,
Bethesda, MD 20892-1504
Tel: 301-594-5789
Fax: 301-402-0244
Molly.Freimuth@nih.gov
QUICK LINKS:
![]()
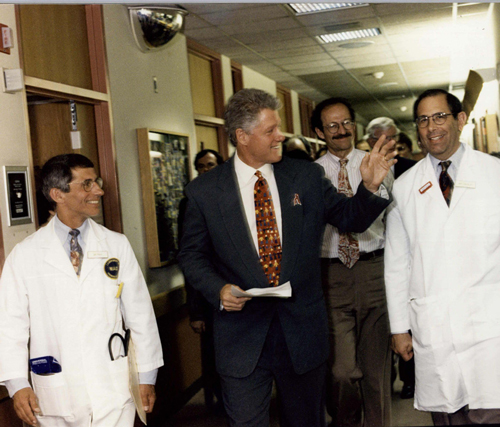
Gallin appointed to new leadership position
| ||
| ||
|
Duties designed to strengthen strategic planning, prioritization, scientific review
For more than two decades, while under the leadership of director Dr. John I. Gallin, the NIH Clinical Center achieved scientific advances that are saving hundreds of thousands of lives, pioneered countless patient-centered initiatives and trained the next Gastroitestinal Tract Seminar
Feb. 7, 2017, Noon — 1:30 p.m.
Lipsett Amphitheater
Presented by Dr. Wendy Garrett, Harvard School of Public Health.
Rare Disease Day at NIH [disclaimer]
Feb. 27, 2017, 8:30 a.m. — 3:30 p.m.
Masur Auditorium
Sponsored by the NIH National Center for Advancing Translational Sciences and Clinical Center, Rare Disease Day raises awareness about rare diseases, affected patients and research collaborations addressing rare disease challenges. Event will feature presentations, posters, exhibits and an art show.
Aging and Inflammation Seminar
Feb. 28, 2017, Noon — 1:30 p.m.
Lipsett Amphitheater
Presented by Connie Weyand, Stanford Medicine.
NOTE: PDF documents require the free Adobe Reader.