CC Grand Rounds tackles workplace culture – generating respect and safety in the clinical research environment
How should medical and scientific research establishments deal with unprofessional behavior by employees? How can this be spotted and dealt with before causing additional conflict?
These questions along with related issues were tackled head-on in the July 24 Clinical Center Grand Rounds address by Dr. Jo Shapiro, Associate Professor in Otolaryngology, Head and Neck Surgery at Harvard Medical School. Directly relevant to the topic of her talk, Shapiro founded the Center for Professionalism and Peer Support at Brigham and Women's Hospital in 2008 and served as its director for 10 years.
What is workplace culture?: Stressing the importance of staff cooperation, peer support and understanding as shared goals, Shapiro began by pointing out some behaviors of disruptive employees and why this behavior has in some cases been ignored, or at least tolerated in the workplace culture. Shapiro says some define workplace culture as an "evolving pattern of behaviors in teamwork, professionalism, and responses to errors and adverse events."
Further defining professionalism as "that which supports trustworthy relationships" Shapiro cited studies showing that up to 5% of personnel in medical and research environments demonstrate unprofessional behaviors that interfere with patient care, and overall quality of service.
And harassment remains – often targeting students and residents. A meta-analysis of over 30 studies across the nation showed that over half of medical students and residents report either discriminatory behaviors or outright sexual harassment, "This should have been over long ago,' stated Shapiro. "We have face it straight on."
The Joint Commission speaks up for safety: Issuing an alert, the Joint Commission clearly states all of its credentialed institutions are to be dedicated to ending "behaviors that undermine a culture of safety" including dismissive or intimidating interaction through inappropriate verbal responses, body language or threatening physical actions.
The role of leadership in establishing a culture of safety: Shapiro stated that organizational leadership must exhibit the same behaviors and the same accountability expected of staff to support institutional excellence. "We've been slow in acknowledging this – everyone needs to be held accountable. Expertise, technical competence and organizational standing are not excuses for ignoring bad behavior," she said.
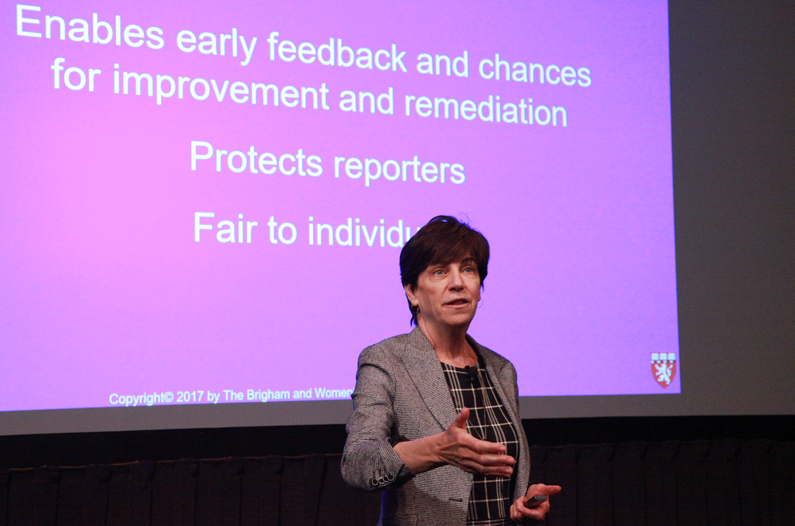
Early intervention matters: Essential to improving workplace culture is a process where early identification of problems is encouraged, with methods fair to all involved so that raising concerns is not avoided for fear of retribution or other negative responses. "Let's make it easy for people speak up and do the right thing," Shapiro stated.
Mistakes happen, but what happens next?: When adverse events and errors occur, a realistic response depends on avoiding the instinctual 'shame and blame', reactions, instead choosing full disclosure, event analysis including open discussion, and sharing lessons learned with colleagues. Finally, resilience, or ability to 'bounce back' to again function in a confident manner is key. Peer support, including counseling in a group or one-to-one setting helps to restore self-confidence in staff who have been involved in adverse patient care events.
Cornerstones for improving workplace culture and safety: Shapiro's research suggests that an effective working environment in the medical research setting depends on observing what could be called 'house rules'. These are a set of principles and procedures accepted by all parties that serve to maximize a culture of trust and cooperation among staff and trainees to support the goal of optimal patient care in the medical setting.
- Robert Burleson